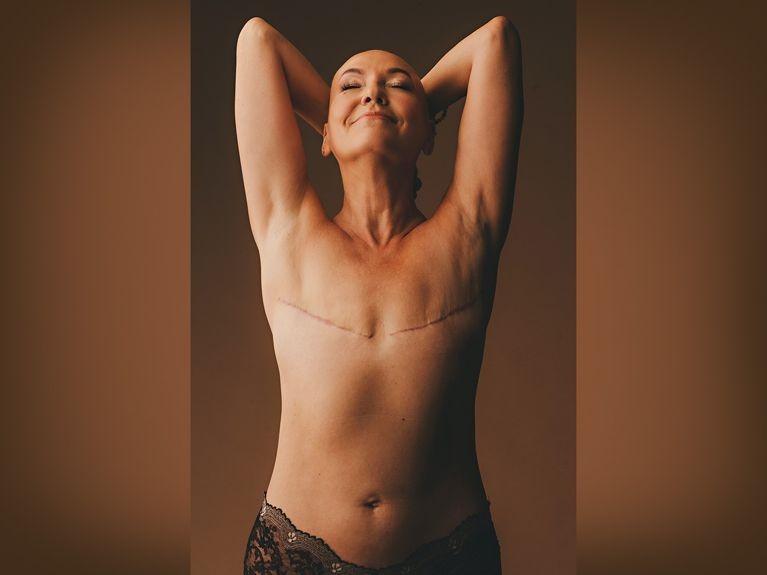
While women often choose to have breast reconstruction after a mastectomy, an increasing number of them are opting for a different path: they are going flat.
The official term for this–as adopted by the National Cancer Institute in 2020–is aesthetic flat closure (AFC). When survivors pick this option, they have the extra skin, tissue and fat in the breast area removed. What’s left of the chest is then tightened and smoothened to issue permanently flat. An expert on this subject is Stacey Sigman, founder of the Flat Retreat which is a community-supported organization that hosts retreats and cultural events for women who choose AFC. And, in this position, she’s been made privy to the many reasons why women choose this procedure.
Sigman said that breast cancer can strip individuals of their sense of control over their bodies. Choosing to go flat, she claimed, is a way to regain that control. It allows survivors to define their beauty standards and embrace their bodies as they are, scars and all.
But AFC also has practical advantages. Breast cancer reconstruction can be complex as it often requires multiple surgeries and a lengthy recovery period. Going flat, on the other hand, is a simpler, less invasive option. It eliminates the discomfort and potential complications associated with breast implants. It also offers a more straightforward path to recovery.
Furthermore, choosing to go flat avoids the risks of breast reconstruction surgery. These include infection, implant rupture, and even the need for additional surgeries to correct complications.
Sigman had her own reasons for going flat. After being diagnosed with breast cancer in 1997, she opted for a single mastectomy followed by chemotherapy. She got diagnosed again in 2013, so she decided to follow the same game plan that she had during her first battle with breast cancer.
“Like most, I followed protocols and listened to my doctors,” she shared. However, her decision to go flat was clear from the start. “I had no desire to create a breast mound that I could not feel,” she said. “I received pushback from my surgeon and plastic surgeon, who thought I would regret it. Regret was never my experience.”
Eventually, Sigman went on social media and found that there were a lot of women who felt the way she did. And, among them, she found not just a community she eventually took part in nurturing.
The rise of the Flat Retreat
The flat community is a group of women who have chosen AFC after mastectomy. It has deep historical roots, encompassing courageous women like Betty Ford, Audre Lorde, Shirley Temple, and Deena Metzger—women who chose to go flat and proudly share their stories long before the era of social media. Nowadays, the flat community–which Sigman has become a part of–is a diverse collective of patients, advocates, activists, doctors, grassroots nonprofits, and supporters who come together to share their personal experiences related to mastectomy.
The group is present in various public and private social media platforms. But, Sigman decided that they should expand beyond cyberspace. Ergo, the Flat Retreat was created.
Conceived in 2019, the Flat Retreat was created to provide a physical gathering for women who chose AFC. The inaugural retreat brought 40 women from across the United States and Canada to a desert location in Palm Springs, California. During the event, the group participated in a local breast cancer walk that went viral after Flat Retreat participants took off their shirts during the march.
Since the Flat Retreat’s inception, the aim has been to create gatherings that would honor and destigmatize living flat. It was also made for its members to share experiences that foster support, and advocate for improved standards of care for women with breast cancer.
“Flat Retreat values the truth about breast-implant illness, challenges bias in the medical community to include non-shaming practices, and promotes patient consent for AFC as an equal option,” Sigman shared.
Flat Retreat’s events have created a culture of acceptance and empowerment within the flat community. They showcase influencers, create their fun, celebrate successes, and support organizations challenging biased medical practices.
In 2020, the organization held its first Annual Flat Visibility Awards, broadcasted live on several social media platforms. Subsequently, they hosted formal Flattie Balls, fashion shows, weekend retreats, virtual workshops, and meetups. They co-hosted International Flat Day with Christy Avila. They also directed and edited a short film of patient interviews for the AFC advocacy group Not Putting On A Shirt; this was used for the latter’s patient advocate table at the National Plastic Surgeon Conference in Las Vegas. These events energized the movement, leading to significant achievements.
Aside from the National Cancer Institute’s adoption of the term “aesthetic flat closure,” which provides patients and doctors with the language to discuss going flat, another feat includes the New York State Legislature passing SB S7881 in 2021. This requires insurance to cover the cost of AFC.
Currently, Flat Retreat aims to continue advocating for similar legislation across all states. It also aims to amend the Women’s Health and Cancer Rights Act. But in order to push for these changes, they flat community needed to overcome a few speed bumps.
Shirts off
In the journey of the flat community, one highlight, Sigman shared, was the birth of Stand Tall AFC (STAFC). This national campaign began in response to Flat Retreat’s refusal to sponsor a table at the Palm Springs Breast Cancer Walk after organizers asked participants to keep their shirts on.
“Hearing this washed over me with a deep silence that I will never forget,” she said. “At that moment, I would allow myself to feel what it was like for others to see me without my breasts, how disturbing it might be, and I started to feel shame. How could women choose this?” This incident therefore led her and others in the movement to focus on the importance of visibility and education.
STAFC, co-founded by Sigman and advocate Renee Ridgeley, took the movement to the streets, organizing hundreds of women from the flat community and their supporters to be ambassadors at local breast cancer walks. What they wanted was simple: body positivity and for AFC to be recognized as an equal option after mastectomy.
STAFC is now in its third year, working alongside Not Putting On A Shirt, and has doubled in size. Meanwhile, women from the flat community continue to support breast cancer walks, with shirts off and brochures in hand to educate participants about AFC.
Reshaping the narrative
As Flat Retreat celebrates its 5th anniversary in Palm Springs, Sigman and the flat community look forward to participating in the Breast Cancer Walk to push for AFC as a valid post-mastectomy option. They will also host a retreat in San Francisco to support the 5th Anniversary of International Flat Day and a retreat in Miami to support STAFC’s final Breast Cancer Awareness Month Walk.
According to Sigman, the decision to go flat is not a rejection of femininity or beauty, but rather redefining it. AFC challenges societal norms and expectations surrounding women’s bodies and beauty standards. As more survivors choose AFC, the narrative of what it means to be beautiful and whole is shifting. The growing movement to normalize this option empowers women to make choices that align with their values and comfort. And, while it is an ongoing journey that may hit a few bumps along the way, many of the prominent people behind it have proven that challenges tend to push them to forward.
The Good Latch: Why the Love for Breast Milk Lasts
Back in 2021, when a highly infectious virus came to a home in Bulacan, Philippines, signs of illness were seen on all of its residents except one: a six-month old baby–he who was supposed to be the most vulnerable person in the house.
It was a case observed by Dr. Kim Ticman-Mapua, a pediatrician tapped to be the lactation expert of the baby’s mother. According to Dr. Mapua, the child’s mom started feeling unwell but she initially thought that she just had “the regular flu.” She therefore didn’t distance herself from her son; she kept playing with him, kissing him and breastfeeding him. But, after five days since she began to feel sick, she lost both her sense of taste and smell. Her housemates—composed of her mother and two children older than her newborn—also started feeling ill.
Recounting this story for PWR, Dr. Mapua reveals that the family contracted the coronavirus disease 2019 (COVID-19.) And, while it was with them, it caused a variety of symptoms that ranged from fever to diarrhea to bodily weaknesses. But while all of this was happening, the baby exposed to his mother didn’t show symptoms. He remained playful, his appetite was promising, and even though he didn’t have a fully developed immune system at that time, he seemed generally well.
As a breastfeeding advocate certified by the International Board of Lactation Consultant Examiners, Dr. Mapua speculates that this may have been due to breast milk.
“Breast milk is like the first vaccine of your baby,” she tells PWR. And to her, this child is but one of the many who stand as testaments to its potency.
The “breast” option
For centuries, humanity has encountered many factors that now influence the way by which we care for children. These include advancements in technology, shifts in culture and the development of new techniques. But, even after the numerous changes we’ve experienced, breast milk, according to health experts, remains to be what’s “best for babies.”
Take, for example, what happened in recent years. When COVID-19 began infecting people at an alarming rate, lives were greatly altered. “Pandemic” became a household term, phrases like “social distancing” and “new normal” were popularized and people were encouraged by medical experts to stay distant from each other. But, in the midst of these changes, the most reputable figures in medicine didn’t discourage the consumption of breast milk often dispensed through the intimate act of breastfeeding; on the contrary, they encouraged it even more.
According to the Center for Disease Control and Prevention (CDC,) breast milk is a rich source of nutrition for infants. The organization states that aside from satisfying a baby’s hunger, its contents can also protect a child from long and short-term illnesses that include asthma, obesity, type 1 diabetes, and sudden infant death syndrome. It also comes free for a lot of mothers, a food supply that puts little to no financial burden on families. What truly makes it remarkable, however, is adaptability—the fact that it can be modified by a mother’s body to be more relevant to the circumstances she is dealing with.
“It changes in real time,” Dr. Mapua tells PWR, supporting the CDC claim. “A mom with a premature baby produces milk for a premature baby. And if there’s an infection ongoing in the family, the mother produces milk with antibodies and she makes it available for her baby.”
This was especially relevant during the height of COVID-19. As explained by the CDC, available research suggests that the breast milk of mothers who have the virus contain antibodies that may “provide immunological protection to infants.” Additionally, most studies supported by the organization indicate that the virus cannot infect the child via breastfeeding so long as the mother practices preventative measures. These include washing up before the feeding process and wearing a mask while a baby feeds.
”That’s the power of breast milk,” Dr. Mapua says. But even with such “power,” there are valid reasons as to why it doesn’t always get chosen by moms.
Breastfeeding “formula”
Breastfeeding is widely considered by experts to be the healthiest and most natural way to feed a child. But, that shouldn’t suggest that it’s easy. For some, the process can be a lot harder than serving a convenient bottle of commercially prepared infant formula which has been advertised to have vitamins and nutrients useful for children. They may not have the antibodies of breast milk but they can satisfy a baby’s appetite without putting moms through the hardships that often accompany breastfeeding.
The process of lactation, after all, is complex. It is an elaborate symphony of sensory impulses and hormonal reactions which tells a body to start producing milk (because of pregnancy) and continue production (in response to frequent and efficient milk removal.) Among the basic principles governing it is the idea that so long as a mother continues to breastfeed, her body will likely continue to produce milk.
According to Dr. Mapua, a lot of elements can disrupt this ideally harmonious operation. And, when they do, that can lead to difficulties that make breastfeeding unattractive.
Anatomical conditions, she says, are among them. Some mothers simply do not have the physical capacity to produce a sufficient supply of breast milk. There are also those who don’t produce any at all. Others, meanwhile, have undergone medical or cosmetic breast-related procedures that make lactation difficult if not impossible.
Environmental factors also impede proper lactation. Stress for instance can be a problem. “Stress inhibits oxytocin, the hormone that is there for milk ejection,” Dr. Mapua says. And to breastfeeding mothers, that can come from a variety of factors: the pressure to produce milk, concern for her baby’s health, the list can go on. This is why some mothers who want to breastfeed can require mental health support from loved ones, licensed professionals and breastfeeding support groups. This is also the reason why partners of lactating moms are encouraged to shoulder some of her day-to-day responsibilities while she focuses on feeding.
To Dr. Mapua, however, one of the worst impediments to successful breastfeeding is misinformation. Up to this day, there are many myths about the process that can lead to the failure of one’s feeding goals. For example, there are mothers with misinformed breastfeeding methods. There are some, she says, who do not know that they have to pump or express their milk in between feedings to create a personal milk bank they can tap when needed and encourage their body to continue milk production. There are also moms who don’t have proper technique. This could lead to a poor latch and that can cause inefficient milk removal or injury which, in turn, can lead to cases like mastitis. A poor latch can also cause unnecessary pain.
This too, is a common subject of misinformation. As Dr. Mapua states, many mothers are led to believe that pain (especially the protracted kind) is natural in breastfeeding. As a result, some moms would just bear with it instead of seeking the help of a specialist. That shouldn’t be, she stresses.
“Majority of cases suggest that pain is not normal,” she shares. “It could mean that there’s something going on.” But a mother, she says, may never know for sure unless she seeks help from experts.
“They don’t have to endure pain,” she declares. “They just need help and good advice.”
They also need to be easy on themselves, she adds. Sometimes, moms who wish to breastfeed fail to achieve their feeding goals. Because of this, they can get discouraged from trying again or they feel bad over their perceived failures. As a mom, Dr. Mapua normally tries to lift their spirits up by reminding them that every parenting journey is different. And, for those who failed to breastfeed a child but wish to try again for their next kid, she has good news.
“I tell them that there are studies suggesting that mothers tend to have more milk for their second baby compared to their first because the body has long-term memory,” she says. “The mammary glands, they form long-term memory during pregnancy. They remember what they need to do so they produce more milk.”
In other words, this discussion returns to the subject of adaptability. This trait is what makes breast milk attractive but it isn’t just an attribute of breast milk per se. It is also a human quality. It is, after all, the body which adapts, alters the milk’s composition to satisfy pressing needs.
In essence, breast milk, according to experts, is good because it can be a platform to express the human capacity to adapt. And, that is a quality with proven merit. The ability to change when needed is the reason why the human race manages to respond adequately to problems. It is the foundation of our capacity to greatly influence the state of the planet. It is also the reason why a global pandemic can happen, cause all sorts of pr oblems but eventually leave many of us with the ability to claim that we are well.
The Bumps in the Road for Travelers Receiving Breast Cancer Treatment
The road to recovery can occasionally lead people away from where they want to be.
This is a common experience of those who want to travel while being treated for breast cancer.
Generally, people with this disease can journey through long distances and a lot of them do. For starters, there are those who have to travel out of necessity; those who live in remote or underdeveloped areas whose lives require a fair amount of border crossing. Meanwhile, there are those who travel for mental wellness; those who take trips for the sake of pleasure to get the frame of mind they need to cope with their condition.
Cancer, however, is a complicated disease. Its treatment—normally long and extensive—is a journey in its own right. And, those who take it can at times find themselves weighed down or even rendered temporarily unfit to go elsewhere.
The trouble with treatment
According to the National Cancer Institute of the United States, cancer happens when “some of the body’s cells grow uncontrollably.” It is because of this growth that they can disrupt and damage vital organs and cause a host of complications that can be debilitating if not fatal. Adding to its complexity is the fact that while these cells begin confined in their area of origin, they can eventually divide and spread to other parts of the body especially when left unchecked. Because of this, it has long been modern medicine’s goal to find these cells (preferably in their early stages) so that they can be removed, killed or at least subdued.
This, however, is the problem: to effectively deal with cancerous cells, the methods used on them are normally quite aggressive. The earliest form of treatment, for example, involves opening people up; one of the newest among them, meanwhile, involves adding new genes to a patient’s cells. Both of these (and other forms of treatment in between) can cause side effects that may leave the body in a weakened state.
According to Cancer Research UK (CRUK,) a known consequence of cancer treatment involves blot clots. The disease, according to them, can already cause these on its own. They say that it may be because cancer cells release chemicals that encourage excessive coagulation. Cancer treatment, however, doesn’t automatically reduce the likelihood of them happening.
Through hormone therapy, for example, doctors use tamoxifen, a drug known to increase the risk of blood clots. Meanwhile, according to Breast Cancer Now, surgery and chemotherapy “can damage the walls of blood vessels.” This can increase the risk of clots developing.
On its website, CRUK says that people who are planning a trip while dealing with cancer treatment should be cautious because travel can also increase the risk of unhealthy blood coagulation.
“Sitting for long periods also increases your risk of developing a blood clot,” says the group. “You need to take care if you’re traveling by car, plane, train or coach. The risk increases on journeys that are over four hours.”
And this is something to be taken seriously, medical experts say. Clots, after all, can block the healthy flow of blood. They can also break off and travel to vital organs and cause a list of complications like strokes and heart attacks. This is why it’s imperative for those at risk of blood clots to protect themselves.
“Take short walks as often as possible,” CRUK says. When riding a plane, a quick, hourly stroll down an aisle will help. In a car ride, meanwhile, it is advised for patients to occasionally stop the vehicle so that they can step out and stretch. Other tips from CRUK include doing simple leg exercises “every hour if you can’t move around much.” They also advise people with cancer to wear compression stockings measured to fit them. Constant hydration through non-alcoholic drinks and wearing loose clothing are also advised. The group also says that patients should consult their doctor before going on trips as they might be instructed to hold off for a few weeks or be prescribed anticoagulants to further prevent blood clots.
“Tell your doctor or nurse straight away if you have pain, swelling or tenderness in one area of your leg, warm or red skin in one area, shortness of breath [and] chest pain.” CRUK says. These may be symptoms of a clotting problem.
In line with that, those undergoing cancer treatment should also speak to their medical team if they’re experiencing the following: fever, sore throat, chills and sweats, nausea, vomiting, diarrhea and various types of pain and discomfort. These might be symptoms of another problem faced by people being treated for cancer: infection.
According to Breastcancer.org, people receiving cancer treatment may be taking medicines that weaken the immune system. Measures that involve these include chemotherapy, certain targeted therapies, high-dose corticosteroids, and surgery. Additionally, certain treatments like surgery and radiation therapy can damage lymph vessels and increase a patient’s risk of developing lymphedema. This is an abnormal swelling that happens when the lymphatic system can’t clear fluid fast enough. This too can lead to infection in the areas swollen by the condition.
In response to this, Breastcancer.org and their contemporaries say that people being treated for breast cancer should exercise what the world has learned during the pandemic to protect themselves. Avoid large crowds if possible. Wear a mask. Practice good hygiene, and be up to date on vaccinations as recommended by their physicians.
Of course, there is a more effective method of avoidance recommended by experts: to wait, to delay travel until one’s doctor believes that they are more than fit enough to do so. But, there are those who may find this difficult.
Determining the Destination
According to the World Health Organization, breast cancer is the most prevalent cancer in the globe. In 2020 alone, about 2.3 million women were diagnosed with it and around 685,000 of those who have it died. In various platforms, people are warned of its dangers and those who genuinely speak about their experiences with it rarely ever refer to the disease as anything less than “life-changing.”
“After a cancer diagnosis, a person’s perspective often changes,” says writer Bonnie Annis. She shares her bout with the disease in the online resource Curetoday.com. There, she explains that “as survivors go through this process, some feel an overwhelming desire to tackle bucket lists at record speed.” This is why people dealing with cancer can sometimes feel the need to rush, to promptly do what they want and visit the places that align with their desires.
The road to recovery doesn’t always go there directly. Sometimes, it takes people through side trips, longer routes and even detours. But, as experts have pointed out, this path doesn’t just lead people away from some of the things that they want; it can also keep them away from a number of things that they don’t.